Spinal fractures are among the most serious injuries patients can face, often leading to pain, disability and reduced independence. While surgical treatment carries upfront costs, its economic value lies in preventing long-term complications that require extensive rehabilitation, home care or assisted living. Dr. Larry Davidson, an advocate for minimally invasive procedures, has emphasized that when fractures are stabilized effectively through surgery, patients are far less likely to become dependent on costly, ongoing care.
By evaluating the financial impact of surgical repair compared with conservative management, it becomes clear that investment in surgery often saves both patients and healthcare systems significant costs in the long run. Beyond financial value, surgery improves quality of life, allowing patients to maintain independence, return to work and reduce reliance on social support systems.
The Cost of Untreated or Poorly Managed Fractures
When spinal fractures are not stabilized effectively, patients face long-term disability. Chronic pain, deformity and neurological deficits can limit mobility and independence, increasing the likelihood of requiring assisted living or long-term care facilities.
Indirect costs such as lost productivity, inability to work and reliance on family caregivers further add to the economic burden. For healthcare systems, repeated hospitalizations, ongoing therapy and pain management become significant expenses. Preventing these outcomes is one of the primary economic arguments for timely surgical intervention.
Upfront Costs vs. Long-Term Savings
Surgical treatment of spinal fractures requires investment in hospital stays, operating rooms, implants and recovery care. These costs may seem high at first glance, compared with bracing or conservative management. Yet studies consistently show that the savings from preventing disability outweigh the upfront expense.
When fractures are repaired surgically, patients are more likely to return to work, maintain independence and avoid prolonged rehabilitation. Long-term savings include reduced reliance on nursing homes, fewer re-hospitalizations and lower spending on pain management. The economic model reflects not just immediate costs, but the lifetime value of restored function.
Preventing Disability Through Stabilization
The primary way surgery delivers economic value is by preventing disability. Stabilizing fractures reduces pain, restores alignment and protects neurological function. It allows patients to walk, perform daily activities and participate in rehabilitation.
Dr. Larry Davidson explains, “Investing in surgical repair can prevent long-term disability and reduce the need for extended care, saving both patients and the healthcare system significant costs.” His perspective highlights that beyond the immediate benefits of stabilization, timely surgery helps patients maintain independence, return to work and rely less on long-term support, making it a smart choice, both medically and economically.
Patients who avoid paralysis or severe deformity remain capable of living independently, reducing long-term reliance on costly support systems. Each case of preserved mobility represents not only a medical success but a financial one, as it reduces the need for ongoing institutional care.
Reduced Need for Long-Term Care
Nursing homes and assisted living facilities represent major costs for patients and healthcare systems. For those with untreated or poorly managed fractures, loss of independence often makes such placements necessary. Surgery significantly lowers this risk by providing stability and restoring function. Patients who undergo effective surgical repair are more likely to remain at home, supported by outpatient therapy, rather than institutional care. This difference translates into thousands of dollars in savings per patient annually.
The Role of Rehabilitation in Cost Savings
Rehabilitation is a key factor in maximizing the cost-effectiveness of surgery. By stabilizing fractures surgically, patients are able to participate more fully in physical therapy, leading to faster and more durable recoveries. Active participation in rehabilitation reduces secondary complications, such as muscle wasting, pressure ulcers and infections, all of which are costly to treat. Surgery provides the foundation, but rehabilitation transforms that foundation into functional, long-term savings.
Advances in Minimally Invasive Techniques
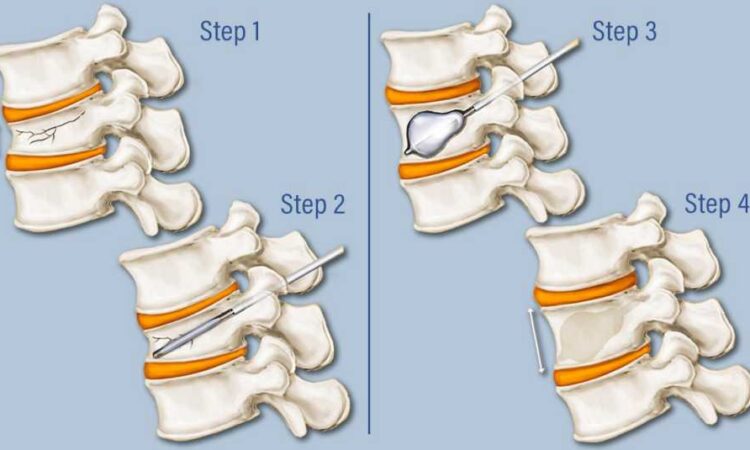
Minimally invasive fracture surgeries, such as percutaneous screw placement and cement augmentation, reduce hospital stays and lower complication rates. Shorter recovery times translate into quicker returns to work and independence, amplifying the cost-effectiveness of surgical treatment. These techniques also reduce the need for prolonged pain management, and limit the likelihood of costly revision surgeries. As technology advances, the economic value of surgical care continues to increase.
Athletes and Cost Considerations
Athletes who sustain spinal fractures present unique cost-effectiveness questions. Surgery not only restores mobility but also protects careers and performance potential. For professional athletes, preserving spinal health may prevent the loss of income that results from early retirement. Even for recreational athletes, returning to activity reduces healthcare utilization, by preventing complications from inactivity. The benefits extend beyond individual patients, to broader healthcare systems that face reduced long-term burdens.
Public Health Perspective
From a public health perspective, spinal fracture surgery helps reduce disability across populations. By decreasing the prevalence of chronic spinal conditions, it lowers demand for rehabilitation centers, long-term care facilities and disability programs. Investing in surgical infrastructure and training allows these benefits to reach more people. The resulting societal cost savings are significant, making access to surgery a priority for both economic and health reasons.
Patients as Partners in Cost-Effective Care
Patient participation is critical in realizing surgery’s economic value. Adhering to rehabilitation programs, maintaining bone health and preventing future fractures all contribute to long-term savings. Surgery alone cannot achieve cost-effectiveness. It depends on a collaborative approach in which patients, surgeons and care teams work together to reduce risks and strengthen outcomes.
Future advancements in biologics, AI planning and smart implants are expected to boost the cost-effectiveness of spinal fracture surgery. By lowering complication rates and improving fusion success, these technologies can shorten recovery times and reduce the need for revision procedures. For patients, this translates to safer surgeries and better protection against long-term disability. For healthcare systems, it directs resources toward interventions that deliver the greatest overall value.
The cost-effectiveness of spinal fracture surgery lies in its ability to prevent disability, reduce reliance on long-term care and restore independence. While upfront costs are significant, the long-term savings in healthcare expenditures and productivity make surgical intervention an economically sound choice. The perspective underscores that spinal surgery must be evaluated not only by clinical outcomes, but by its economic impact. This approach reflects a vision of care that preserves both health and financial stability for patients and society.




